In a groundbreaking study, our group has uncovered how a small protein on the surface of a gut-dwelling bacterium, Brachyspira pilosicoli, could hold the key to understanding some troubling intestinal conditions. This bacterium is notorious for causing intestinal spirochetosis, which is linked to symptoms like diarrhea, abdominal pain, and weight loss.
The Culprit: BPP43_05035
At the heart of the discovery is a protein called BPP43_05035, which acts as an "adhesin" – a sticky molecule that allows bacteria to latch onto cells in the gut lining. Think of it as Velcro for bacteria! But its role goes beyond simple attachment.
Using advanced tools like protein structure mapping and cell culture experiments, postdoc Anandi Rajan found that this protein doesn't just stick to the cells lining the gut; it also targets tight junctions, the cell "gatekeepers" that maintain the integrity of the intestinal barrier. By weakening these tight junctions, BPP43_05035 increases the permeability of the gut lining, allowing harmful substances and bacteria to potentially seep through.
Why Does This Matter?
The gut lining is essential for health, acting as a protective barrier against harmful microbes while letting in nutrients. When this barrier is compromised, it can lead to conditions like irritable bowel syndrome (IBS) or even systemic infections.
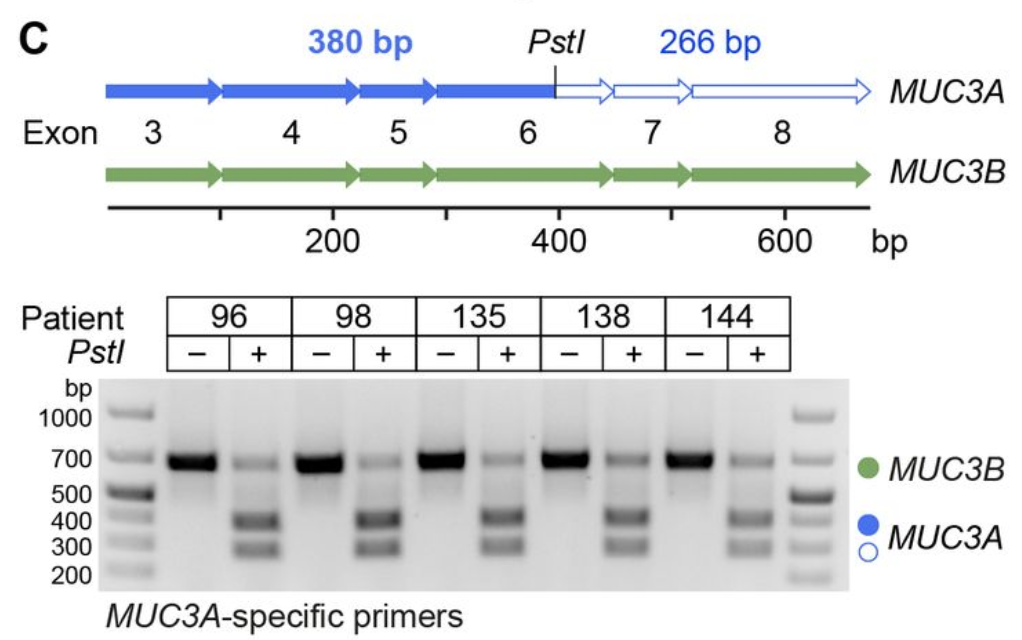
Our study also revealed that in patients infected with Brachyspira pilosicoli, certain protective genes in the gut lining are less active. This means the bacteria and its adhesin, BPP43_05035, could play a role in chronic gut disorders.
A Glimmer of Hope
There’s exciting potential here for medical science. Blocking the function of BPP43_05035 with specific antibodies stopped the bacteria from attaching to gut cells in lab experiments. This opens the door for targeted therapies to prevent or treat infections caused by Brachyspira pilosicoli.
What’s Next?
This discovery is a significant step toward understanding how bacteria interact with our gut. Future research will aim to develop interventions that can block bacterial adhesins like BPP43_05035 and restore gut health in affected patients.
Understanding this tiny but mighty protein could lead to big advances in managing gut health and tackling persistent infections!
Read the paper at Gut Microbes.